Prostatitis
Prostatitis is one of those things that guys might not want to talk about, but it’s more common than you’d think. It’s basically an inflammation of the prostate gland. This tiny gland, about the size of a walnut, sits right below the bladder and plays a big part in male health. When it acts up, you might feel pain when you pee, or even in your lower back or groin. Sometimes it’s caused by a bacterial infection, but not always. It’s important to figure out what’s going on because the symptoms can really mess with your day-to-day life.
Key Takeaways
- Prostatitis is an inflammation of the prostate gland that can cause pain and urinary issues.
- There are different types of prostatitis, including bacterial and non-bacterial forms.
- Symptoms can include difficulty urinating, pelvic pain, and sometimes flu-like symptoms.
- Diagnosis often involves a physical exam and tests to rule out infections.
- Treatment can vary from antibiotics to lifestyle changes, depending on the type.
Understanding Prostatitis
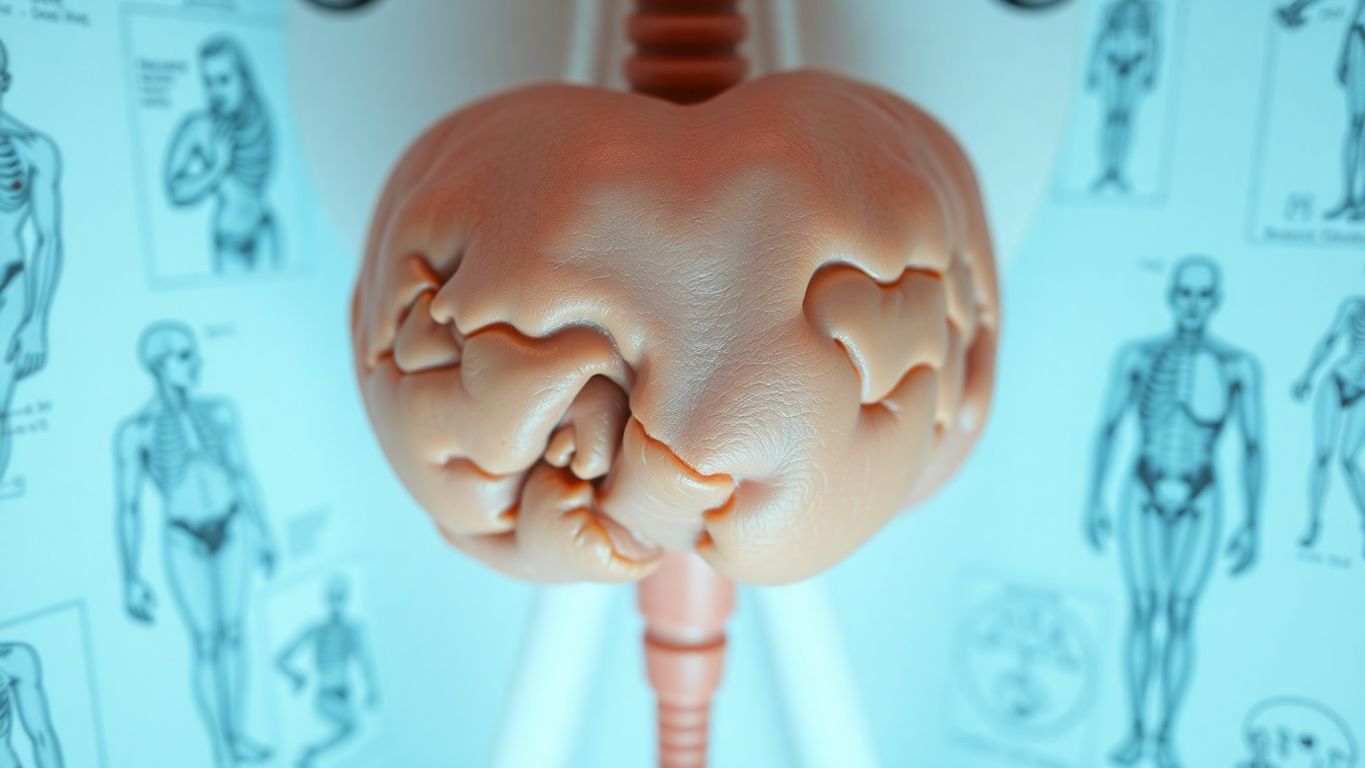
Definition and Overview
Prostatitis is a condition involving inflammation of the prostate gland, which is located just below the bladder in men. This gland is about the size of a walnut and plays a role in producing seminal fluid. Unlike prostate cancer, prostatitis is not a form of cancer but can cause significant discomfort and urinary issues. It often leads to painful urination, pelvic pain, and discomfort in the genital area. While some cases are due to bacterial infections, others are not, making diagnosis and treatment a bit tricky.
Types of Prostatitis
There are four main types of prostatitis:
- Acute Bacterial Prostatitis: This type is caused by bacterial infection and comes on suddenly with severe symptoms like fever, chills, and urinary problems.
- Chronic Bacterial Prostatitis: A persistent bacterial infection that may have milder symptoms but can recur.
- Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS): The most common type, characterized by pelvic pain and urinary symptoms without a clear infection. Chronic prostatitis can affect quality of life significantly.
- Asymptomatic Inflammatory Prostatitis: Inflammation of the prostate without symptoms, often discovered incidentally during tests for other conditions.
Common Symptoms
Symptoms of prostatitis can vary depending on the type but generally include:
- Pain or burning sensation when urinating
- Difficulty urinating, such as dribbling or hesitant urination
- Frequent need to urinate, especially at night
- Pain in the lower back, groin, or at the tip of the penis
- Discomfort during or after ejaculation
Prostatitis can often mimic symptoms of other conditions, such as urinary tract infections or even symptoms related to prostate cancer, making it important to seek medical advice for an accurate diagnosis. Early detection and treatment can help manage symptoms effectively and improve quality of life.
Causes and Risk Factors of Prostatitis
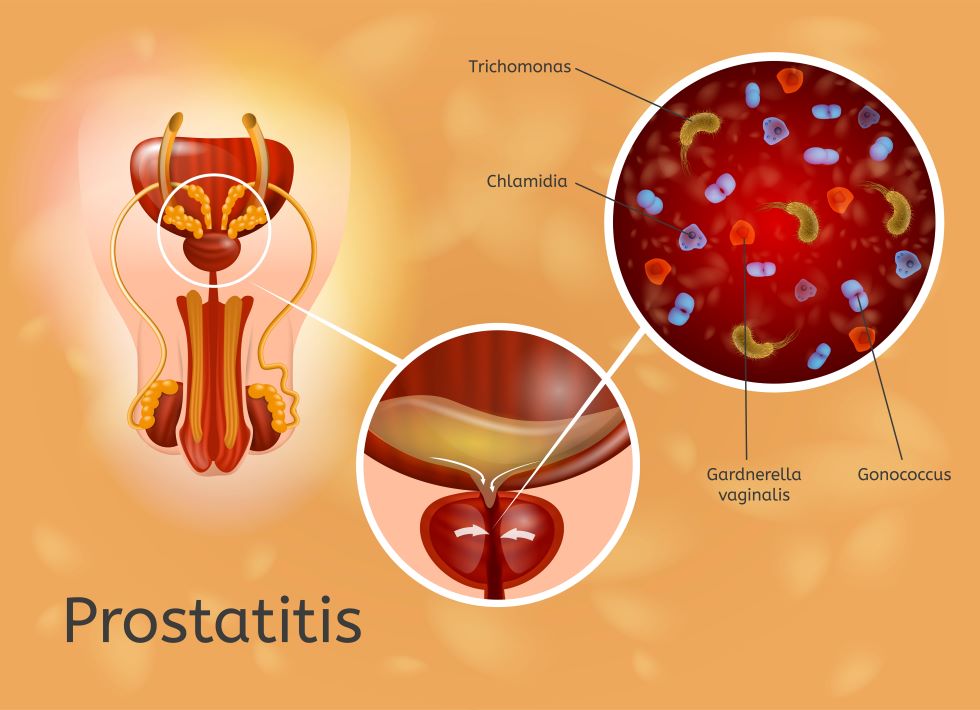
Bacterial Infections
Prostatitis can often be traced back to bacterial infections. These pesky bacteria might sneak into the prostate via the urethra or when urine flows backward. Some common culprits include bladder infections, bladder stones, or sexually transmitted infections (STIs). Using a urinary catheter or having a prostate biopsy can also open the door for bacteria. In many cases, the bacterial forms of prostatitis come from infections that spread from other areas of the urinary or reproductive systems.
Non-Bacterial Causes
Not all prostatitis cases stem from bacteria. Chronic pelvic pain syndrome (CPPS) and nonbacterial prostatitis are different beasts. Potential contributors to these conditions include autoimmune diseases, pelvic floor muscle damage, pelvic nerve irritation, or even stress. It’s tricky because these types don’t have the straightforward bacterial cause, making them a bit of a mystery.
Risk Factors
Certain factors can increase the chances of developing prostatitis. Being young or middle-aged is one of them. A history of sexually transmitted diseases can also be a risk factor, as well as having a previous bout of prostatitis. If you’ve had frequent urinary tract infections (UTIs) or an abnormal urinary tract, you’re more at risk. Other risk factors include:
- HIV infection or AIDS
- Use of a urinary catheter
- Diagnostic procedures involving the prostate, like a biopsy
- Psychological stress or nerve damage in the pelvic region
Understanding these causes and risk factors can help in managing and preventing prostatitis, though it’s not always a straightforward path. Sometimes, the cause remains elusive, adding to the complexity of dealing with this condition.
Living with prostatitis can be challenging, but recognizing the risk factors and causes is a step towards better management and possibly preventing future episodes.
Diagnosing Prostatitis
Physical Examination
Diagnosing prostatitis often begins with a visit to your healthcare provider, who will likely start with a physical examination. During this exam, a digital rectal exam (DRE) is commonly performed. This involves the doctor inserting a lubricated, gloved finger into the rectum to feel the prostate gland for any swelling, tenderness, or abnormalities. This simple procedure helps to identify inflammation or pain in the prostate area.
Laboratory Tests
Laboratory tests are crucial for confirming a diagnosis of prostatitis. One of the key tests is a urine culture, which involves analyzing a urine sample to detect the presence of bacteria and white blood cells. This test is particularly important for diagnosing chronic bacterial prostatitis. Additionally, a blood test might be conducted to check for signs of infection or other prostate issues. In some cases, a prostate massage might be performed during the DRE to release prostate fluid into the urethra, which is then expelled in a urine sample for further testing.
Imaging Techniques
If initial tests are inconclusive, imaging techniques may be employed to get a clearer picture of the prostate and surrounding areas. A transrectal ultrasound is a common method used to visualize the prostate gland and identify any abnormalities, such as abscesses or stones. In some instances, a CT scan might be used to provide detailed images of the pelvic region, helping to rule out other potential causes of symptoms. These imaging methods are valuable tools in pinpointing the exact nature of the problem and guiding further treatment options.
Diagnosing prostatitis can sometimes be a bit of a process, involving multiple tests and evaluations. But getting an accurate diagnosis is key to finding the right treatment and getting relief from symptoms.
Treatment Options for Prostatitis
Antibiotic Therapy
When it comes to prostatitis, antibiotics are often the go-to treatment, especially for bacterial forms. If you have acute bacterial prostatitis, you might find yourself on a course of antibiotics for two to four weeks. It’s crucial to complete the entire course to ensure the infection is fully cleared and to prevent antibiotic resistance. In more stubborn cases of chronic bacterial prostatitis, treatment can extend from four to twelve weeks. Sometimes, if the infection is particularly persistent, a low-dose antibiotic regimen might be prescribed long-term to keep it at bay.
Pain Management
Pain can be a real burden with prostatitis, so managing it is a big part of treatment. Over-the-counter pain relievers like ibuprofen or acetaminophen can help. For those with more severe pain, prescription medications might be necessary. Some folks find relief through alternative methods like acupuncture or biofeedback, which can help manage chronic pain by teaching you to control certain body responses. If stress and anxiety are part of the equation, therapy or counseling can be beneficial too.
Surgical Interventions
Surgery isn’t the first line of defense for prostatitis, but in rare cases, it might be considered. If there’s an abscess that needs draining or if the prostate is causing significant urinary issues, surgical intervention might be necessary. For chronic bacterial prostatitis that doesn’t respond to medication, surgery to remove part or all of the prostate could be an option, though this is quite uncommon.
Living with prostatitis can be challenging, but understanding your treatment options and working closely with your healthcare provider can make a significant difference in managing the condition.
Living with Prostatitis

Lifestyle Modifications
Living with prostatitis means making some changes to your daily routine. Adjusting your lifestyle can really help manage the symptoms. Here are a few tips to consider:
- Stay Hydrated: Drink plenty of water throughout the day. It helps flush out bacteria and keeps your urinary system functioning well.
- Limit Alcohol and Caffeine: These can irritate your bladder and worsen symptoms, so it’s best to cut down.
- Exercise Regularly: Gentle exercises like walking or swimming can improve blood flow and reduce tension in the pelvic area.
Support and Resources
It’s important not to face prostatitis alone. There are resources and support systems that can help you cope:
- Join Support Groups: Connecting with others who have similar experiences can provide comfort and practical advice.
- Seek Professional Guidance: Don’t hesitate to reach out to healthcare professionals for advice tailored to your situation.
- Educational Materials: Access brochures and books that offer detailed insights into managing prostatitis.
Managing Flare-Ups
Flare-ups can be frustrating, but knowing how to handle them can make a big difference:
- Identify Triggers: Keep a journal to track activities or foods that seem to trigger symptoms.
- Pain Management: Over-the-counter pain relievers like ibuprofen can ease discomfort during a flare-up.
- Rest and Relaxation: Take time to rest and use relaxation techniques such as deep breathing or meditation to ease stress.
Living with prostatitis requires patience and understanding. It’s not always easy, but with the right approach and support, managing it becomes more bearable. Remember, you’re not alone in this journey, and seeking help is always a good step forward.
For more information on how lifestyle changes can impact prostatitis, consider exploring studies that document these effects.
Prevention and Prognosis

Preventive Measures
Preventing prostatitis isn’t always straightforward, but there are some steps you can take to lower your risk. Here’s what you should consider:
- Safe Sexual Practices: Always use protection, like condoms, to reduce the risk of sexually transmitted infections which can lead to prostatitis.
- Prompt Treatment of UTIs: If you suspect a urinary tract infection, get it treated quickly to prevent it from spreading to the prostate.
- Regular Check-Ups: Visiting your healthcare provider regularly can help catch any early signs of prostatitis, allowing for timely intervention.
Long-Term Outlook
Living with prostatitis can be challenging, but with proper management, many find relief from symptoms. Most cases of bacterial prostatitis respond well to antibiotics, often within a few weeks, though chronic cases might require longer treatment. Acute prostatitis is treated with antibiotics for 2 to 6 weeks, while chronic prostatitis requires a longer course of antibiotics, also lasting at least 2 to 6 weeks. For non-bacterial prostatitis or chronic pelvic pain syndrome, treatment might focus on symptom relief and lifestyle changes.
It’s important to stay in communication with your healthcare provider to ensure your quality of life isn’t affected as you manage prostatitis.
When to Seek Medical Help
Don’t hesitate to contact your doctor if you notice any of the following:
- Persistent pain in your lower back, pelvis, or genitals.
- Difficulty urinating or pain during urination.
- Symptoms like fever, chills, or feeling generally unwell.
Being proactive about these symptoms can lead to better outcomes and prevent complications. If you’re unsure about your symptoms or how to manage them, seeking medical advice is always a good step.
Taking care of your prostate is important for a healthy life. To help you stay on track, we invite you to visit our website for tips and products that can support your prostate health. Don’t wait—start your journey to better health today!
Wrapping Up on Prostatitis
So, prostatitis is a bit of a mixed bag, isn’t it? It can hit anyone, anytime, and the symptoms can be all over the place. From needing to pee all the time to feeling like you’re on fire when you do, it’s no walk in the park. The good news is, there are treatments out there. Antibiotics are the go-to for bacterial types, but sometimes you might need a bit more, like a massage or even surgery. It’s not something you can catch from someone else, but it can be linked to other infections. If you’re dealing with any of these symptoms, it’s best to see a doctor sooner rather than later. They can help figure out what’s going on and get you on the right track. Remember, taking care of your health is always worth it.
Frequently Asked Questions
What is prostatitis?
Prostatitis is when the prostate gland, which is a small gland in men located below the bladder, gets inflamed or swollen. It can make peeing hurt or feel difficult, and sometimes it causes pain in the lower belly or private parts.
What are the common symptoms of prostatitis?
The symptoms can include a burning feeling when you pee, needing to pee often, pain in the lower back or belly, and sometimes fever or chills. It can also hurt when you sit down or when you have a bowel movement.
How is prostatitis diagnosed?
Doctors usually check for prostatitis by asking about your symptoms and doing a physical exam. They might also test your urine or blood to look for signs of infection.
What causes prostatitis?
Prostatitis can be caused by bacteria getting into the prostate, but not always. Sometimes the cause is unknown, and it can be linked to stress or past infections.
How is prostatitis treated?
Treatment depends on what type you have. Doctors might give you antibiotics if it’s caused by bacteria. They might also suggest medicine to help with pain or inflammation.
Can prostatitis be prevented?
While you can’t always prevent prostatitis, staying healthy by drinking plenty of water and practicing good hygiene can help. Avoiding activities that could injure the area can also reduce risk.